Introduction
The uncommon neurological disorder known as intracranial hypertension, sometimes known as pseudotumor cerebri, is characterized by increased pressure inside the skull. The condition can be perplexing and challenging to diagnose, which commonly leads to missed diagnoses and subpar treatment. We will look at the causes and risk factors for intracranial hypertension in this post to help us comprehend this mysterious illness.
1. What is Intracranial Hypertension?
Intracranial hypertension, at its heart, is a medical disorder marked by increased pressure surrounding the brain and spinal cord. Numerous symptoms, including as severe headaches, visual abnormalities, and pulsatile tinnitus, may be brought on by the elevated pressure.
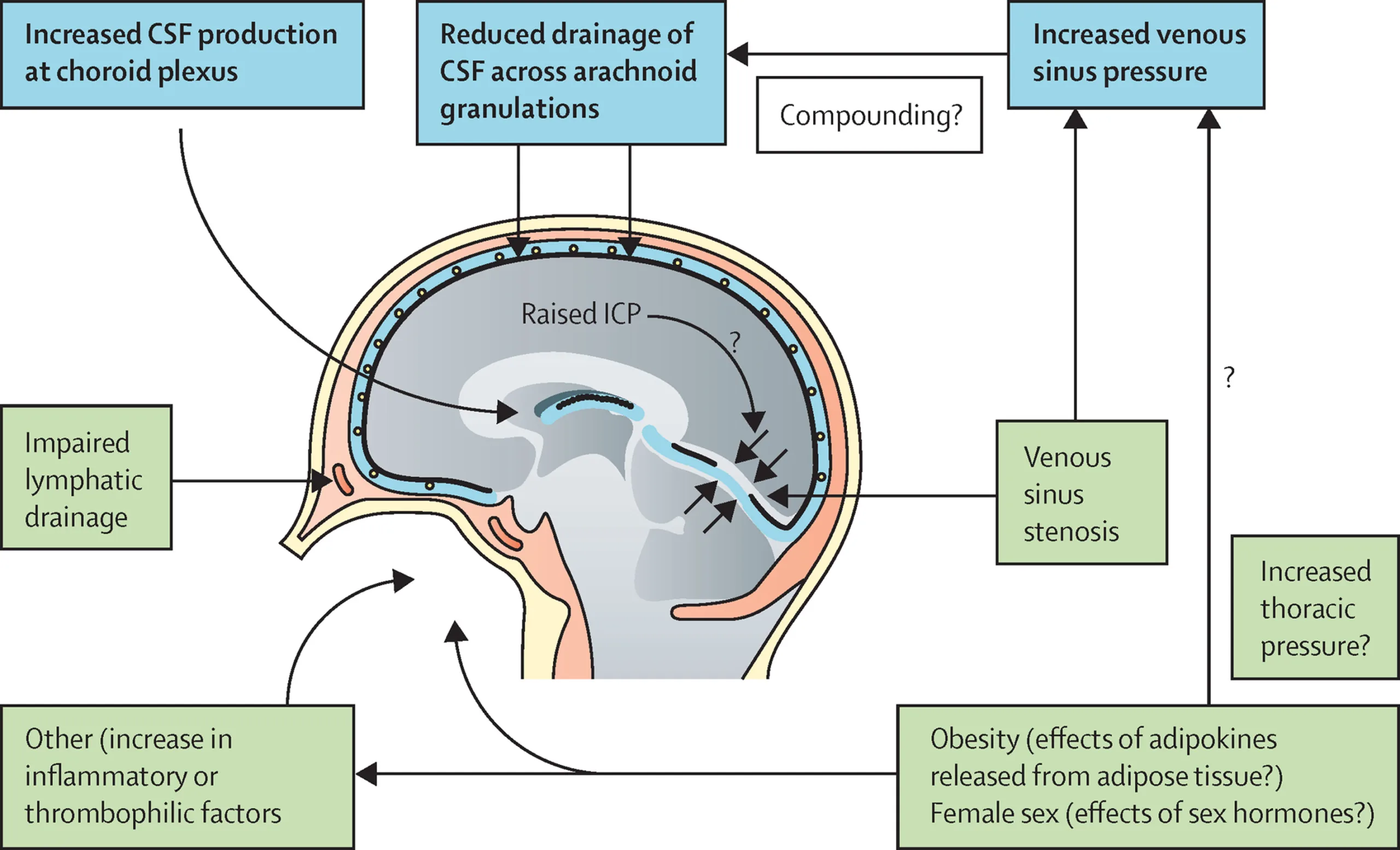
2. Understanding the Mechanism
The exact mechanism behind intracranial hypertension is not yet fully understood. However, one prevailing theory suggests that the condition may occur due to an imbalance in the production and absorption of cerebrospinal fluid (CSF). CSF is a clear, protective fluid that surrounds the brain and spinal cord.
3. Potential Causes
Several factors can contribute to the development of intracranial hypertension. Some common causes include:
3.1. Obesity
Obesity has been linked to an increased risk of developing intracranial hypertension, particularly in young women. Excess adipose tissue can lead to hormonal changes and affect CSF dynamics.
3.2. Certain Medications
Certain medications, such as tetracycline antibiotics, growth hormones, and some contraceptive pills, have been associated with intracranial hypertension as a potential side effect.
3.3. Head Trauma
A history of head trauma or brain injury can also predispose individuals to intracranial hypertension.
3.4. Cerebral Venous Sinus Thrombosis
In rare cases, the condition may be triggered by cerebral venous sinus thrombosis, a condition where blood clots form in the venous sinuses within the brain.
4. Risk Factors
While the exact cause remains uncertain, several risk factors have been identified that may increase the likelihood of developing intracranial hypertension:
4.1. Age and Gender
The condition primarily affects women of childbearing age, though it can occur in men and individuals of any age.
4.2. Chronic Illnesses
Certain chronic illnesses, such as sleep apnea, kidney disease, and thyroid disorders, have been linked to an increased risk of intracranial hypertension.
4.3. Family History
A family history of intracranial hypertension may predispose an individual to the condition.
4.4. Vitamin A Toxicity
Excessive intake of vitamin A, either through supplements or specific medications, may contribute to the development of intracranial hypertension.
5. Symptoms and Diagnosis
The symptoms of intracranial hypertension can vary from person to person. Common signs include:
- Persistent headaches, often worse in the morning or upon bending over.
- Visual disturbances, such as double vision or temporary blindness.
- Ringing in the ears (pulsatile tinnitus).
- Nausea and vomiting.
- Neck stiffness.
6. Seeking Medical Attention
If you experience any of the symptoms mentioned above, it is essential to seek prompt medical attention. Early diagnosis and treatment can help prevent further complications.
7. Diagnosis
Diagnosing intracranial hypertension can be challenging, as its symptoms can mimic other neurological conditions. A comprehensive evaluation may involve:
7.1. Neurological Examination
A thorough neurological examination is typically the first step in the diagnostic process.
7.2. Eye Examination
An eye examination, including visual field testing, is crucial to assess potential optic nerve damage.
7.3. Lumbar Puncture
A lumbar puncture, also known as a spinal tap, may be performed to measure CSF pressure.
7.4. Imaging Studies
Brain imaging studies, such as MRI or CT scans, can help rule out other structural abnormalities.
8. Treatment Options
Treatment for intracranial hypertension aims to alleviate symptoms and reduce intracranial pressure. Depending on the severity and underlying cause, options may include:
8.1. Weight Management
For patients with obesity-related intracranial hypertension, weight management through diet and exercise may be recommended.
8.2. Medications
Certain medications, such as diuretics and acetazolamide, can help reduce CSF production and lower intracranial pressure.
8.3. Optic Nerve Sheath Fenestration
In severe cases, where vision is at risk, surgical procedures like optic nerve sheath fenestration may be considered to relieve pressure on the optic nerve.
9. Lifestyle Modifications
Adopting certain lifestyle changes can complement medical treatment and improve overall well-being. These may include:
9.1. Limiting Sodium Intake
Reducing sodium intake can aid in fluid balance and reduce CSF production.
9.2. Managing Caffeine Intake
Caffeine consumption should be moderated, as it can contribute to fluid retention.
9.3. Regular Exercise
Engaging in regular physical activity can support weight management and promote overall health.
Conclusion
Intracranial hypertension remains an enigmatic condition, but advancements in medical research continue to shed light on its causes and risk factors. Early diagnosis, along with appropriate treatment and lifestyle modifications, can significantly improve the quality of life for those affected by this condition.
FAQs About Intracranial Hypertension
Q1. Is intracranial hypertension a life-threatening condition? Intracranial hypertension can lead to serious complications if left untreated. Prompt medical attention and appropriate management can prevent potential risks.
Q2. Can men develop intracranial hypertension? While the condition primarily affects women, men can also develop intracranial hypertension.
Q3. Can intracranial hypertension be cured completely? While there is no definitive cure, proper treatment can manage symptoms effectively and improve the patient’s condition.
Q4. Can intracranial hypertension cause permanent vision loss? Without timely intervention, intracranial hypertension can lead to permanent optic nerve damage and vision loss.
Q5. Are there any preventive measures for intracranial hypertension? Maintaining a healthy lifestyle, managing chronic illnesses, and seeking medical attention for symptoms can reduce the risk of developing intracranial hypertension.